OVERVIEW: Psoriasis is a chronic, inflammatory autoimmune skin disease that causes red, scaly patches to appear on the skin.
It usually affects the outside of the elbow, knee, or skull, although it can appear at any location. Some people report that psoriasis is itching, burning, and stinging. Psoriasis is connected with other serious health conditions, such as diabetes, heart disease, and depression.
Plaque psoriasis is one of the usual common forms. The flare-up of psoriasis can be initiated by some environmental trigger.
Psoriasis is not contagious. It becomes better and worse spontaneously and may periodically cause remission (clear skin).
It can be controllable with medication, but not curable. There are several promising new treatments, including new biological drugs.
If you develop a rash that does not go away with an over-the-counter medication, you should consider contacting your doctor.
What are the symptoms and signs?
Its Symptoms and signs vary for everyone. Symptoms range from mild to severe and may present differently depending on the type of psoriasis.
Common signs and symptoms include:
- Rashes or patches of red, swollen skin, usually covered with loose, silver-colored scales. In severe cases, plaques will grow and absorb into each other, covering wider areas.
- In some people, it has been observed that psoriasis causes itching or soreness. Itchy, painful skin that may crack or bleed
- Small areas of bleeding where the affected skin is scratched
- Problems with your fingernails and toenails, including discoloration and tiredness; Nails may also begin to dislodge or detach from the nail bed.
- Scalic plaques on the skull.
There are many different types of psoriasis. Many have only 1 form at a time, although there may be 2 different types simultaneously. One form may change to another or be more severe.
Most cases of psoriasis go through a cycle, reducing problems for a few weeks or months. Periods on average last 1–12 months at a time.
However, both the time period and the relaxation period can be challenging to predict.
According to the National Psoriasis Foundation:
- Mild psoriasis covering less than 3% of the body
- Moderate psoriasis covering 3-10% of the body
- Severe psoriasis covering more than 10% of the body.
What are the causes and risk factors?
The exact cause is unknown, with scientists believing it to be an autoimmune disease. A combination of elements including genetic predisposition and environmental factors is involved.
Psoriasis is common in members of the same family. The immune system is thought to play a major role in the control of defects and inflammation.
The cause will be different in every person with psoriasis, but common causes include:
- Stress and anxiety
- Skin injury
- Infection
- Hormonal changes
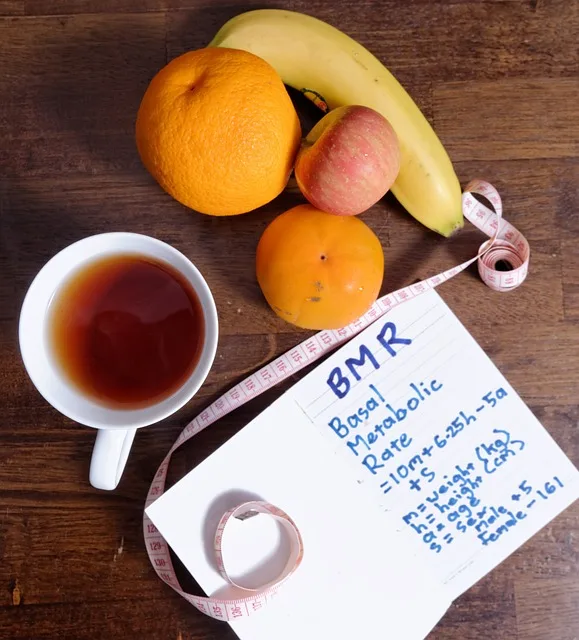
According to one study, about 7.4 million Americans have these diseases. It is usually associated with many other conditions, including:
- Diabetes type 2
- Stomach ache disease
- Kidney disease
- Heart disease
- High blood pressure
- Anxiety
- Depression
- Eye conditions
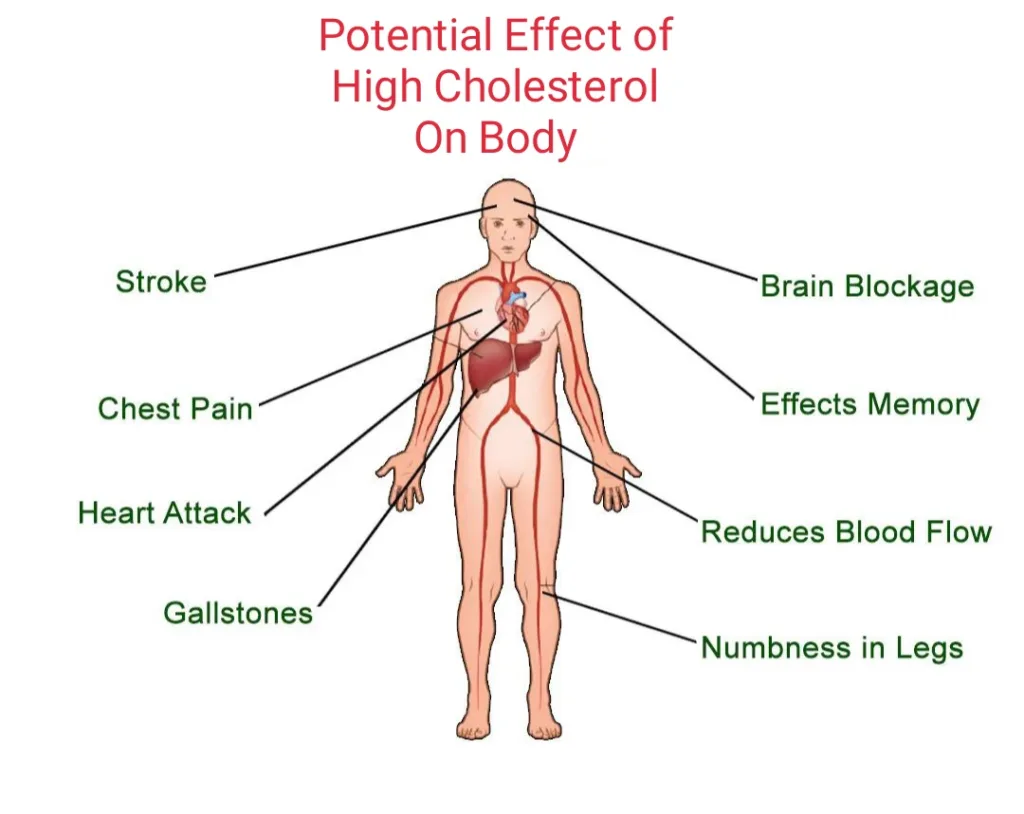
- Obesity
- Metabolic syndrome
- Emotional problems
Medications that can trigger psoriasis include:
- Lithium
- Antimalarials
- Quinidine
- Indomethacin
Some people associate psoriasis with allergies, diet, and weather, but no evidence yet supports these theories.
Importantly, psoriasis is not contagious. Knowing this can help people suffering from the disease to face the more challenging parts of socialization.
What are the types?
Mostly 7 types of psoriasis include:
- Plaque psoriasis
- Nail psoriasis
- Guttate Psoriasis
- Pustular psoriasis
- Inverse Psoriasis
- Erythrodermic Psoriasis
- Psoriatic Arthritis
Knowing what type of psoriasis you have helps you and your doctor in the treatment plan. Most people have only one type at a time. Sometimes, after your symptoms go away, a new form of psoriasis will emerge in response to the trigger.
1. Plaque psoriasis

This is the most common type, plaque psoriasis causes dry, raised, red skin lesions (plaques), covered with silver scales.
About 8 out of 10 people have this type. You can call your doctor this “psoriasis Vulgaris”.
Plaques may be itchy or painful and may be few or many. They can occur anywhere on your body, including your genitalia and the soft tissue inside your mouth.
The American Academy of Dermatology (AAD) estimates that about 80 percent of people have plaque psoriasis. This causes red, inflamed patches that cover skin areas. These patches are usually covered with whitish-silver scales. These plaques are usually found on the elbows, knees, and scalp.
2. Nail psoriasis

It can affect the fingernails and toenails, causing peeling, abnormal nail growth, and discoloration. Half of the people with psoriasis have nail changes.
It is even more common in people who have psoriatic arthritis, which affects your joints. Psoriatic nails may loosen and detach from the nail bed (onycholysis). In severe cases, the nail may rupture.
3. Guttate Psoriasis

This type often starts in children or young adults. It happens in less than 2% of cases. This type of psoriasis causes small pink-red spots on your skin.
They often appear on your:
- Trunk (torso)
- Arms (upper arms)
- Legs (thighs)
- Scalp
These spots are unusually thick or raised like plaque psoriasis. This can go away within a few weeks, even without treatment or you may have repeated episodes.
Some cases, though, are more stubborn and require treatment. It’s usually triggered by a bacterial infection such as strep throat.
4. Pustular psoriasis

This is uncommon and mostly appears in adults. This uncommon form of psoriasis can occur in widespread patches in smaller areas on your hands, feet or fingertips.
It causes white, pus-filled blisters and extensive areas of red, inflamed skin. Usually develops quickly, blisters filled with pus appear just a few hours after your skin becomes red and tender.
The blisters may come and go frequently. Generalized leprosy psoriasis can also cause fever, chills, severe itching, and diarrhea.
These may look infectious but are not. When this happens, it can be very serious, so get medical attention right away.
5. Inverse Psoriasis

This mainly affects bright areas of red, shiny, inflamed skin that worsen with friction and sweating.
Patches of inverse psoriasis develop under:
- Armpits
- Groin
- Under the breast
- Skin folds around the genitals and buttocks (around skinfolds in the genitals).
Fungal infections may trigger this type of psoriasis.
6. Erythrodermic Psoriasis

This type is the least common, but it is very severe, erythrodermic psoriasis can cover your entire body with a red, peeling rash that can itch or burn intensely.
Other symptoms include:
- Severe itching, burning or peeling
- Fast heart rate
- Change in body temperature
The skin is almost sunburned. Scales that often develop are closed into large sections or sheets. It is not uncommon for a person with this type of psoriasis to have a fever or become very ill.
This type can be fatal, so individuals should see a doctor immediately.
7. Psoriatic Arthritis

Psoriatic arthritis is a condition where you have both psoriasis and arthritis (joint inflammation). In addition to inflamed, papular skin, psoriatic arthritis causes inflamed, painful joints that are typical of arthritis.
Sometimes joint symptoms are the first or only manifestation of psoriasis or sometimes only nail changes are seen.
Although the disease is not usually as severe as other forms of arthritis, it can cause stiffness and progressive joint damage that can lead to a permanent deformity in the most severe cases.
In 70% of cases, people have psoriasis for about 10 years before having psoriatic arthritis. It is accompanied by nail changes in about 90% of people.
When do you need to see a doctor?
If you doubt that you may have psoriasis, see your doctor for a test. Also, talk to your doctor if your psoriasis:
- Causes you discomfort and pain
- Makes it difficult to do regular work
- Causes you to worry about the appearance of your skin
- Leads to joint problems, such as soreness, swelling, or inability to perform daily tasks
Seek medical advice if your signs and symptoms worsen or do not improve with treatment. To manage psoriasis, you may need a different medicine or a combination of treatments.
Diagnosing psoriasis
There are no special blood tests or devices for the diagnosis of psoriasis. A dermatologist (a doctor who specializes in skin diseases) or other health care providers usually examine the affected skin and determine if it is psoriasis. 1
Couple tests or examinations may be necessary to diagnose psoriasis. In most cases, the diagnosis of psoriasis is fairly straightforward.
Physical examination and medical history
Your doctor can usually diagnose psoriasis by examining your medical history and your skin, scalp, and nails. Also, tell your doctor if any family members have the condition.
Skin biopsy
If the symptoms are not clear or if your doctor wants to confirm their suspected diagnosis. Then, your doctor may take a small sample of the skin (biopsy).
He will probably apply a local anesthetic first. The specimen is examined under a microscope to determine the exact type of psoriasis and to detect other disorders. It can also detect other possible disorders or infections.
Most biopsies are done in your doctor’s office on the day of your appointment. Your doctor may have injected a local numbing medication to make the biopsy less painful. They will then send a biopsy to a laboratory for analysis.
When the results return, your doctor may request an appointment to discuss findings and treatment options with you.
What are the treatment options?
There is no cure for psoriasis. Therapies or treatment aim to reduce inflammation and scales, slow the growth of skin cells, and remove plaques.
Therapies or treatment can be divided into three main types:
- Topical treatment
- Light therapy, and
- Systemic medicines.
Topical treatment
Used alone, the creams and ointments you apply to your skin can effectively treat mild to moderate psoriasis. When the disease is more severe, the cream may be combined with oral medications or light therapy. Its treatments include:
- Topical corticosteroids
- Topical retinoids
- Calcineurin inhibitors
- Anthralin
- Vitamin D analogues
- Salicyclic acid
- Moisturizer
- Coal tar.
Light therapy (phototherapy)
Ultraviolet (UV) or natural light is used in this treatment. The simplest and easiest form of phototherapy involves exposing your skin to a controlled amount of natural sunlight.
Other forms of light therapy include:
- Artificial ultraviolet A (UVA) or UVB phototherapy,
- Narrowband UVB phototherapy,
- Goekerman Therapy,
- Psoralen Plus Ultraviolet A (PUVA),
- Excimer laser.
Sunlight kills overactive white blood cells that are attacking healthy skin cells and causing rapid cell growth. Both UVA and UVB light can be helpful in reducing the symptoms of mild to moderate psoriasis.
Most people with moderate to severe psoriasis will benefit from a combination of treatments. This type of therapy uses more than one treatment type to reduce symptoms.
Some people may use the same treatment throughout their lives. Others may sometimes need to change treatment if their skin stops responding to the reactions they are using.
If their initial treatment is successful, then people can get phototherapy at home using a lightbox or handheld device.
Some people may need to take psoralen pills before exposure to get their skin further sensitive to light.
Whatever co-existing conditions that make them sensitive to light, such as lupus or previous examples of skin cancer, phototherapy should not be used.
Systemic medicines (Oral or injected medications)
If you have severe psoriasis or are resistant to other types of treatment, your doctor may prescribe oral or injectable medications. This is known as systemic treatment.
People with moderate to severe psoriasis, and who do not respond well to other treatment types, may need to use oral or injected medications.
Due to severe side effects, some of these drugs are used only for brief periods and may be optional with other forms of treatment.
These medicines include:
- Methotrexate
- Cyclosporine (Sandimmune)
- Biology (drugs that alter the immune system)
- Retinoids
- Other medicines: thioguanine (tabloid) and hydroxyurea (droxia, hydria) are medications that can be used when other medicines cannot be given.
Home medications
It is not possible to avoid psoriasis flares, but some strategies may help reduce the risk of a flare-up.
Suggestions include:
- Yoga, exercise, meditation or reducing stress with all of them
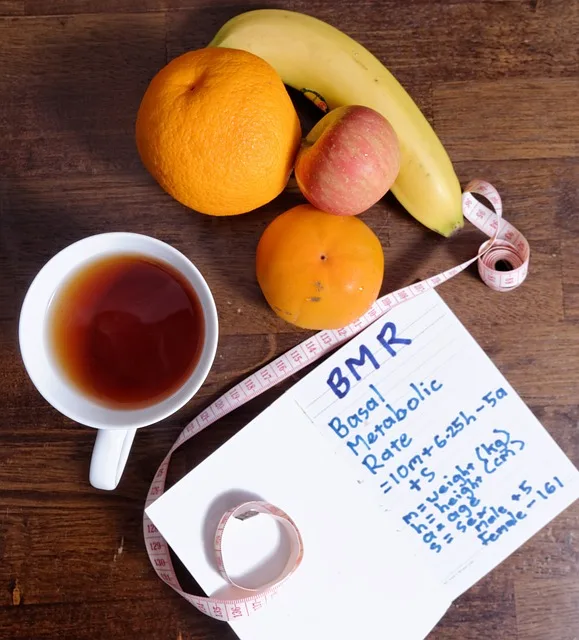
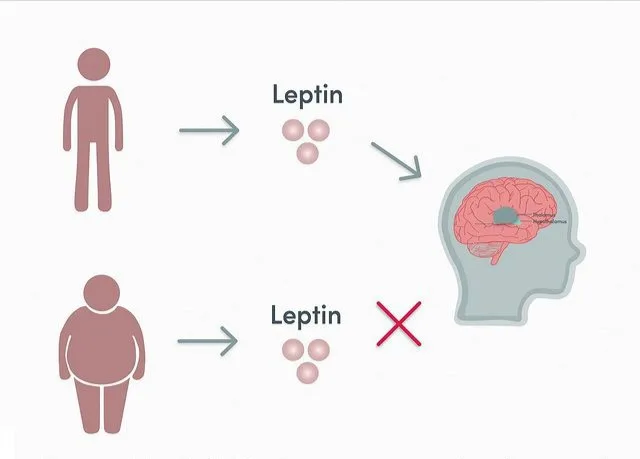
- To have a well-balanced diet and maintain a healthy weight
- Identifying and avoiding food triggers
- Connecting to a support group or blog to talk to others with similar experiences
- Do not smoke or drink too much.
Home remedies to reduce itching include:
- Keep skin moisturized. A dermatologist may recommend an appropriate product.
- Take a cold bath for 10 minutes or use a cold pack. Avoid hot showers, as they can dry the skin
- While psoriasis can be isolated and uncomfortable, people have many options for managing symptoms and treating the immune activity of the disease.
Alternative medicine
Several alternative treatments are claimed to reduce the symptoms of psoriasis, including specialized therapies, creams, dietary supplements, and herbs.
None have been proven to be effective of course. But some alternative treatments are generally considered safe, and they can be helpful in reducing signs and symptoms for some people, such as itching and scaling.
These treatments would be best suited for those suffering from paralysis, erythroderma or arthritis.
Aloe vera: Taken from the leaves of the Aloe Vera plant, aloe extract cream can reduce redness, scaling, itching, and swelling. You may have to use the cream several times a day for one or more times a month to see any improvement in your skin.
Fish oil (Omega-3 fatty acids) supplements may reduce psoriasis-associated inflammation, although results from studies are mixed. Taking 3 grams or less of fish oil daily is generally considered safe, and you may find it beneficial.
Oregon grape, also known as the barberry, topical application of the Oregon grape can reduce inflammation and reduce symptoms of psoriasis.
If you are considering dietary supplements or other alternative medicine to reduce the symptoms of psoriasis, consult your doctor. They can help you weigh the pros and cons of specific alternative treatments.
Avoid trigger foods
Psoriasis causes inflammation. Certain foods cause inflammation too. Avoiding those foods might improve symptoms.
These foods include:
- Red meat
- Refined sugar
- Processed foods
- Dairy products
Drink less alcohol
Alcohol consumption can increase your risks of a flare-up. Cut back or quit entirely. If you have a problem with your alcohol use, your doctor can help you form a treatment plan.
Consider taking vitamins
Some doctors prefer a vitamin-rich diet to vitamins in pill form. However, even the healthiest eater may need help getting adequate nutrients. Ask your doctor if you should be taking any vitamins as a supplement to your diet.
Pregnancy
Psoriasis does not affect fertility, and women with psoriasis may have a normal pregnancy and a healthy baby. Some women have an improvement in their psoriasis during pregnancy, but for others, it worsens.
If you are thinking of having a baby, talk to your health team. Some treatments can be harmful to the developing child, so use contraception while taking them.
It can apply to both men and women depending on the drug. Your healthcare team can suggest the best ways to control your psoriasis before starting a family effort.
Self-care
Self-care is an essential part of your daily life. This includes taking responsibility for one’s own health and well-being, with the support of those involved in your care.
Self-care includes staying fit, maintaining good physical and mental health, preventing illness or accidents, and caring more effectively for minor illnesses and long-term conditions.
People with long-term conditions can benefit greatly from self-care:
- They can last a long time;
- There is less pain, anxiety, depression, and fatigue;
- Have a better quality of life;
- Additionally should be more active and independent.
Having a care plan will help you manage your treatment so that it suits your lifestyle.
Statistics
Psoriasis can begin at any age, but most diagnoses occur in adulthood. The average age of onset is between 15 and 35 years. 2 According to the World Health Organization (WHO), some studies estimate that approximately 75 percent of cases are diagnosed before the age of 46. The second peak period of diagnosis can be in the late 50s and early 60s. 3
According to the WHO, males and females are affected equally. Whites are dissatisfied. People of color diagnose a very small proportion.
Having a family member with the condition increases the risk of developing this disease. However, many people with the condition have no family history. Some people with a family history do not develop this disease.
About one-third of people with psoriasis will be diagnosed with psoriatic arthritis. In addition, people with psoriasis are more likely to develop a condition such as:
- Diabetes type 2
- Kidney disease
- Heart disease
- High blood pressure
Although this data is not exhaustive, research suggests that psoriasis cases are becoming more common. Whether people are developing skin conditions or doctors are only getting better at diagnosing it is not clear.
Speak to others
Many people with this have found that joining support groups helps. Support groups can boost your confidence, reduce feelings of isolation and give you practical advice on how to live with the situation.
- Kim WB, Jerome D, Yeung J. “Diagnosis and management of psoriasis.” Can Fam Physician. 2017 Apr;63(4):278-285. PMID: 28404701; PMCID: PMC5389757. Avalable from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5389757/.[↩]
- Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM; Global Psoriasis Atlas. “National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study.” BMJ. 2020 May 28;369:m1590. doi: 10.1136/bmj.m1590. PMID: 32467098; PMCID: PMC7254147.[↩]
- “Global report on psoriasis.” WHO Library Cataloguing-in-Publication Data. ISBN 978 92 4 156518 9. (NLM classification: WR 205). Available from: https://apps.who.int/iris/bitstream/handle/10665/204417/9789241565189_eng.pdf.[↩]